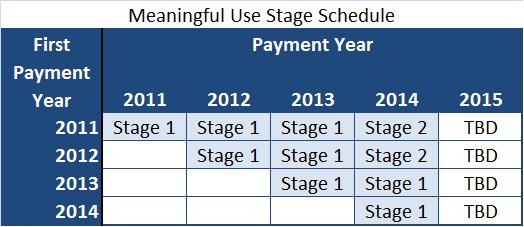
Sifting through the hundreds of pages of new rules can be overwhelming. Luckily, CMS has provided comparison charts to help navigate the meaningful use changes coming our way with Stage 2. Along with the new rules, CMS clarified that the earliest Stage 2 meaningful use is effective is fiscal year 2014 for hospitals and calendar year 2014 for eligible professionals (more on 2014 to come in future posts).
Click on the links below to see the comparison charts:
Stage 2 Meaningful Use – Eligible Professionals: 17 core objectives, 3 of 6 menu objectives, 9 of 64 clinical quality measures.
Stage 2 Meaningful Use – Hospitals & CAHs: 16 core objectives, 3 of 6 menu objectives, 16 of 29 clinical quality measures.
For more information about meaningful use and the EHR Incentive Programs please contact Elana Zana.